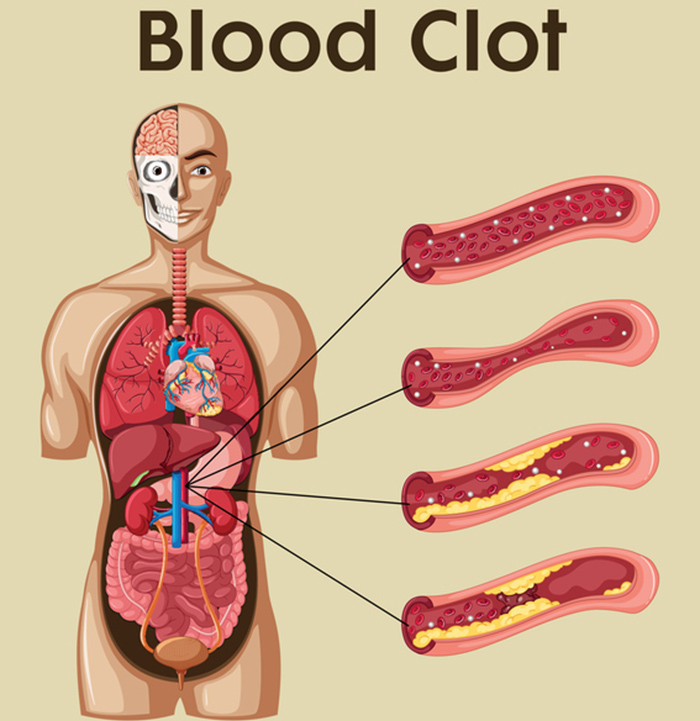
Blood clots can range from mild and easily treatable to very severe. Whatever your situation and urgency may be, it’s important to know your options before starting any medication or your blood clot treatment plan. Blood clots can have a variety of symptoms, depending on where in the body they have formed, so it’s important to know what the various symptoms are and to keep an eye out for them if you suspect you may have a blood clot somewhere. Once a blood clot has been confirmed by a doctor, however, the next step is figuring out the best way to treat it. The blood clot treatments below cover a wide variety of options that you have.
Source: Thinkstock/colematt
Blood clots can be treated with anticoagulants or blood thinners. A blood thinner simply slows the time it takes for your blood to form a clot. They can also be used to prevent clots from happening altogether. There are three common blood thinners which are used for blood clot treatments today: heparin, low molecular weight heparin, and warfarin.
Unfractionated Heparin (UF)
UF heparin is a very fast acting blood thinner. It is taken through an injection under your skin or a needle inserted into a vein through IV. Heparin through an IV works within just a few minutes. If you are in the hospital, you will mostly likely get heparin through an IV. Heparin does need to be monitored daily, so that is something to keep in mind. Your blood will need to be tested every day to make sure you are taking the correct amount.
Blood levels will change sometimes, and when that happens, the amount of heparin you are taking will need to change as well, which is why your blood clot treatment needs to be monitored carefully. An advantage to taking UF heparin is that it does not cost a lot. The cost of meds can end up being a deciding factor for a lot of people, but this form of treatment does have other advantages as well – it gets into your blood quickly, it works fast to prevent clots, and the effect of UF heparin will wear off quickly once the IV drip is stopped.
There are some disadvantages, though; a big one being that it requires daily blood tests. Another big disadvantage is that if you require it in your vein or through an IV, you will have to be hospitalized. Treating a new blood clot can mean up to 10 days in the hospital. Bleeding, skin rash, headache, cold symptoms, and an upset stomach are some the side effects you may experience.
Low Molecular Weight Heparin (LMWH)
LMWH is like UF heparin but you are able to take it at home by giving yourself a shot or an injection under your skin. It also lasts longer in the body than UF heparin and is more predictable so it won’t generally need close monitoring. No need for monitoring means that patients will not need to undergo daily blood tests, which can be a huge relief as daily tests can become a real burden. It is a much more convenient option for sure since you do not need to stay in the hospital in order to take it. One problem with LMWH is that it is more expensive, which can, unfortunately, cause problems for single or low-income families. There is also a higher risk of a condition known as heparin-induced thrombocytopenia, which is a loss of bone strength. This condition is much less likely when taking UF heparin.
Warfarin
Warfarin is a pill you can take for longer-term blood thinning. UF heparin and LMWH are usually only taken for a short term. Your doctor will generally add the warfarin in with whatever heparin you are taking so that you take both of them for a few days as the warfarin must reach a certain level in your blood in order to be effective.
It usually takes around 5-7 days of mixing the two before the warfarin reaches a proper level. The great thing about switching to warfarin is that it can also be taken at home, so once the warfarin reaches a good level, the doctor will stop the heparin and you will be able to go home. Warfarin is an advantageous choice as it is inexpensive and comes in pill form – not shots or injections! Warfarin is also very familiar to doctors as it has been used to treat blood clots in patients since the 1950’s.
Because warfarin increases the time it will take for your blood to clot, you may experience some bleeding. Other side effects of this blood clot treatment may include headache, hair loss, rash, purple toes, skin breakdown, or possible elevated liver enzymes. These side effects will sometimes go away on their own, but if you experience any prolonged side effects or unusual symptoms, you should speak with your doctor right away. Warfarin does require frequent blood monitoring, especially when you first start taking it.
The blood test used to monitor warfarin is called an INR, which stands for an international normalized ratio. The INR measures how long it takes your blood to clot. Most patients do well with an INR between 2.0 and 3.0, which is known as the “therapeutic range,” although some patients may require a higher or lower INR. While these tests can be annoying at first, once your INR is stabilized, you will only need to test your blood about once a month. The tests can be done by going into the lab, or if you prefer, there are finger stick tests that you can use at home -although home testing can be expensive.
It is recommended that you take warfarin at the same time each day, and the evening tends to be the best time because you can change your dose on the same day of your INR if required. If you miss a dose, there is an eight-hour window in which you can still safely take it. If you miss a dose and don’t take it within the eight hours, however, it is recommended that you call your doctor right away.
It is also advised to keep alcohol to a minimum while on warfarin as too much of it can increase your risk of bleeding. When starting on warfarin, or any medication really, it is important that you tell your doctor, nurse, and/or pharmacist about all of the medications that you are on, including herbal and dietary supplements. There are many over-the-counter medications that may increase your risk of bleeding and other side effects. There are also some medications that can change your INR.
Newer Medications
There are some new blood thinners that have been recently approved by the FDA and are now available, like Apixaban, Dabigatran, and Rivaroxaban. These medications are newer and doctors likely won’t be as familiar with them, but they may be more suited to you and your needs. You always want to speak with your doctor first and discuss your situation.
Featured Image Source: Thinkstock/PhonlamaiPhoto